Have you ever considered how your daily food choices might be shaping your mood and mental clarity? This is the central question of nutritional psychiatry, an exciting field exploring the profound link between our diet and mental health. It goes beyond the temporary satisfaction of a good meal, focusing on how specific nutrients can influence our brain’s chemistry and our emotional state.
The concept of ânutritional psychiatryâ is revolutionizing our approach to mental wellbeing. It posits that the food we consume could be a significant factor alongside traditional therapeutic methods. This perspective is steadily gaining recognition from health professionals, researchers at institutions like University College, and the general public.

This article examines the core principles of nutritional psychiatry. We will look at how certain foods and dietary patterns can boost your mood and potentially lessen the symptoms of various mental health conditions, including anxiety. Prepare to learn how your diet could become a powerful tool for improving your mental wellness.
Table of Contents:
- What is Nutritional Psychiatry?
- The Science Behind Nutritional Psychiatry
- Key Nutrients for Mental Health
- The Mediterranean Diet and Mental Health
- The Role of Gut Health in Mental Well-being
- Nutritional Psychiatry in Practice
- Challenges and Limitations of Nutritional Psychiatry
- Tips for Incorporating Nutritional Psychiatry Principles
- The Future of Nutritional Psychiatry
- Conclusion
What is Nutritional Psychiatry?
Nutritional psychiatry is a specialized field that studies the connection between dietary intake and mental health. Its foundation is the scientific understanding that what we eat directly impacts our brain’s structure, chemistry, and function, thereby affecting our mood. This approach uses food as a practical and accessible tool for managing and potentially preventing certain psychiatric disorders.
A primary principle of nutritional psychiatry is the intimate communication between the gut and the brain, known as the gut-brain axis. This pathway means that the state of our digestive system can have a direct effect on our mental state, and the reverse is also true. The field is advanced by organizations like the International Society for Nutritional Psychiatry Research (ISNPR), which advocates for a scientifically rigorous approach.
Researchers focus on how various nutrients influence brain health and how specific dietary patterns might assist with mental disorders. The objective is to integrate these dietary strategies as a complementary aspect of comprehensive mental health care. The field continues to grow as accumulating data suggests a strong association between diet quality and mental health outcomes.
The Science Behind Nutritional Psychiatry
The science supporting nutritional psychiatry is grounded in human physiology and the brain’s high metabolic rate. Our brains depend on a steady stream of nutrients to function correctly, and the quality of that fuel is critically important. Increasing evidence from observational and experimental studies shows that our dietary choices have a substantial impact on our psychological health.
For example, research has demonstrated that diets high in processed foods and refined sugars can exacerbate symptoms of mood disorders and increase the risk for depression. Conversely, whole-food diets rich in nutrients like omega-3 fatty acids appear to have protective benefits for the brain. These findings underscore the significant role our diet plays as one of the determining factors in mental health.
A central player in this biological process is the gut microbiota, the complex community of microorganisms in our digestive tract. This ecosystem is vital for producing neurotransmitters, including serotonin and dopamine, which are fundamental in regulating mood. A disruption in the gut microbiota can influence brain function, highlighting the importance of a healthy diet for a healthy mind.
Key Nutrients for Mental Health
Specific nutrients have been identified as especially crucial for optimal brain function and mental wellbeing. Here are some of the most researched and important components in nutritional psychiatry:
- Omega-3 Fatty Acids: Found in fatty fish like salmon and mackerel, as well as in flaxseeds and walnuts, these fats are vital for brain cell structure and communication. They may help reduce symptoms of depression.
- B Vitamins: This group of vitamins, particularly B12, B6, and folate (B9), helps produce brain chemicals that influence mood. They are also involved in processes that protect brain cells.
- Probiotics and Prebiotics: Probiotics are beneficial bacteria found in fermented foods that support a healthy gut microbiota. Prebiotics are the fibers that feed these bacteria, found in foods like onions, garlic, and bananas.
- Antioxidants: Vitamins C and E, flavonoids, and carotenoids are found in colorful fruits and vegetables. These compounds protect brain cells from oxidative stress, a form of cellular damage.
- Magnesium: This mineral, found in leafy greens, nuts, and whole grains, plays a role in the body’s stress response system and helps promote calmness.
- Zinc: Essential for neurotransmitter function and cognitive health, zinc is found in lean meats, legumes, and seeds.
Incorporating these nutrients through a balanced diet can support your mental health. It is important to focus on a varied dietary pattern rather than isolated nutrients. This holistic approach provides a wider range of health benefits.
The Mediterranean Diet and Mental Health
When discussing dietary patterns that support mental health, the Mediterranean diet consistently receives high praise. This style of eating emphasizes fruits, vegetables, whole grains, legumes, fish, and healthy fats, particularly olive oil. It features low consumption of red meat and processed foods.
Multiple studies, including a landmark randomized controlled trial known as the SMILES trial, have shown that individuals following a Mediterranean-style diet experience lower rates of depression. A key aspect of this dietary intervention is its high diet quality, providing an abundance of nutrients essential for brain health. This dietary pattern is also associated with reduced inflammation, a known risk factor for various mental disorders.
The health benefits extend beyond mental wellbeing, as this diet is linked to lower risks of heart disease, type 2 diabetes, and cognitive decline. This makes adopting a Mediterranean dietary pattern a powerful strategy for improving overall health. The contrast with a Western diet high in processed items and saturated fat is stark and highlights the impact of our food environment.
Mediterranean vs. Western Dietary Patterns
To better understand the differences, consider this comparison of the two dietary patterns and their common components:
| Dietary Component | Mediterranean Diet | Typical Western Diet |
|---|---|---|
| Primary Fat Source | Olive Oil | Butter, Margarine, Processed Vegetable Oils |
| Protein Sources | Fish, Poultry, Legumes, Nuts | High intake of red meat and processed meats |
| Carbohydrates | Whole Grains, Fruits, Vegetables | Refined Grains, Sugary Drinks, Sweets |
| Dairy | Moderate intake, mostly cheese & yogurt | High intake of milk and processed cheese |
| Fruit & Vegetable Intake | High and varied intake daily | Low intake, often processed or fried |
| Snack Foods | Nuts, Seeds, Fresh Fruit | Chips, Cookies, Processed Snack Bars |
The Role of Gut Health in Mental Well-being
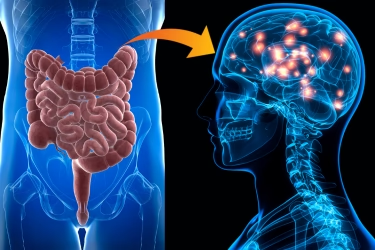
The gut-brain connection is a foundational concept in nutritional psychiatry. Our digestive system contains an intricate neural network, often called the “second brain,” due to its profound influence on our mental and emotional state. The gut microbiota produces a significant portion of the body’s neurotransmitters that regulate mood and stress resilience.
A healthy and diverse gut microbiota is essential for mental health. When these trillions of bacteria are imbalanced, a condition known as dysbiosis, it can lead to chronic inflammation. This inflammation is not confined to the gut; it can affect the entire body, including the brain, potentially contributing to mental health issues like depression and anxiety.
A diet rich in fiber from plants, fermented foods like yogurt and kefir, and a wide variety of whole foods helps cultivate a flourishing gut microbiota. Such dietary strategies directly support a healthy gut, which in turn promotes better mental health. This connection shows just how much our food choices matter for our daily feelings and long-term wellbeing.
Nutritional Psychiatry in Practice
How does nutritional psychiatry translate into everyday life? It functions as a complementary approach rather than a replacement for conventional mental health treatments. A professional trained in this field, perhaps at a leading medical center, collaborates with therapists and doctors to build a complete treatment plan.
This approach begins with a thorough evaluation of an individual’s current diet, lifestyle, and health history. Based on this assessment, a practitioner might suggest specific dietary strategies tailored to the person’s unique needs. This could involve adding nutrient-dense foods, limiting items like processed foods that can negatively affect mood, or shifting the overall dietary pattern.
It’s vital to recognize that nutritional psychiatry is not an overnight solution. Similar to other mental health approaches, achieving results requires consistency, patience, and commitment. The positive effects of dietary changes on mood and mental wellbeing accumulate over time.
Challenges and Limitations of Nutritional Psychiatry
While nutritional psychiatry holds significant promise, it faces several challenges. A primary obstacle is the difficulty of nutrition research. It can be hard to conduct a scientifically rigorous study that isolates the precise effects of individual nutrients or a complex dietary pattern on mental health.
Another challenge is that individual responses to dietary changes can vary widely. Factors like genetics, lifestyle, body composition, and overall health status can all shape how a diet affects an individual’s mental state. This means a one-size-fits-all approach is not effective, and personalized guidance is often necessary.
Furthermore, there is a risk of overstating the role of diet in mental health. While diet is a powerful modifier, it is just one component of the complex mental health picture for conditions like major depressive disorder. Stress levels, genetics, socioeconomic status, and life experiences are also critical determining factors.
Tips for Incorporating Nutritional Psychiatry Principles
If you wish to apply the principles of nutritional psychiatry to improve your own mental health, here are some practical tips to begin:
- Focus on Whole Foods: Build your meals around a wide variety of whole foods, including a rainbow of fruits and vegetables to maximize antioxidant intake.
- Include Omega-3 Sources: Add fatty fish like salmon to your weekly routine, or incorporate plant-based sources such as flaxseeds, chia seeds, and walnuts.
- Reduce Processed Items: Consciously limit foods high in added sugars, refined grains, and unhealthy fats, as these can contribute to inflammation and mood swings. A poor diet is a significant risk factor.
- Support Your Gut: Include fermented foods like yogurt, kefir, sauerkraut, or kimchi to introduce beneficial probiotics and support your gut microbiota.
- Stay Hydrated: Dehydration can directly impact concentration and mood, so ensure you drink plenty of water throughout the day.
Remember, these dietary shifts should support, not substitute, any ongoing mental health treatments. Always talk with a healthcare professional before making substantial alterations to your diet, especially if you are managing a health condition.
The Future of Nutritional Psychiatry
As the evidence base for nutritional psychiatry expands, we can expect to see greater integration of dietary approaches into standard mental health care. More information is becoming readily available, and a quick search for a pmc article or a free pmc article will yield a wealth of studies. This could result in more personalized treatment plans that combine traditional therapies with targeted nutritional interventions.
There is also growing momentum to apply these principles to public health policies for improving mental health on a larger scale. Could government dietary guidelines be revised to better support mental wellbeing? Can we use food as a primary prevention tool to reduce the incidence of psychiatric disorders?
These are important questions that researchers are actively investigating through an increasing number of controlled trials. As our understanding of the intricate links between diet and mental health deepens, we may witness a fundamental shift in how society approaches mental wellness. This research continues to be published in journals like Eur Neuropsychopharmacol and discussed by leading academics.
Conclusion
Nutritional psychiatry offers an empowering perspective on mental health care, highlighting that our wellbeing is deeply connected to what we eat. While it is not a cure-all, it provides invaluable insight into how we can actively support our mental health through conscious dietary choices. This approach is more than a trend; it’s a return to understanding food as a foundation of health.
As the field matures and research continues to build the evidence base, our understanding of how specific foods and dietary patterns affect brain function and mood will become even clearer. In the meantime, adopting a balanced, nutrient-rich dietary pattern is a positive and proactive step we can all take. It is a key part of a holistic strategy for improving mental health.
It’s important to view nutritional psychiatry as one component in a comprehensive mental health toolkit. It is most effective when used alongside other evidence-based approaches, such as therapy and medication when appropriate. By embracing a holistic view of mental health that includes diet, we create more pathways to achieve lasting wellness.


0 Comments